Written by Katie Emmett, Education and Training Manager at Physiquipe
Presented by Anicia Baron, an Occupational Therapist and a Hand Specialist based at Pulvertaft Hand Centre
Injury to the hand resulting in a contracture can lead to many problems. This type of injury can interfere with the functional use of the hand so treatment can be vital. Instrument Assisted Soft Tissue Mobilisation (IASTM) is an effective manual therapy treatment that can be used to treat a range of soft tissue injuries to the hand. Establishing the best treatment approach and having a range of treatment options for specific injuries can be vital in rehabilitation.
Proximal interphalangeal (PIPJ) joint flexion contractures, or loss of extension at the middle joint of the finger, can occur after injury, disease and surgery and can interfere with the functional use of the hand. Scar tissue contributions from the surgical incision, bulky repairs and biomechanics of the hand working with short levers, especially the little finger adds to the complications of a joint contracture and can be extremely problematical to treat.
Anicia Baron, an Occupational Therapist and a Hand Specialist based at Pulvertaft Hand Centre presents a treatment case study for a PIP joint contracture following a flexor tendon repair.
Patient background:
- 33 year old male with HX of mental health problems
- 31/05/2020 - knife injury to R dominant little finger
- 100% division of Flexor Digitorum Supericialis (FDS) and Flexor Digitorum Profundus (FDP)
- 09/06/2020 - surgery (delayed due to COVID-19)
- Repair FDP (FDS not repaired to facilitate smooth tendon glide)
Therapy intervention:
- 10/06/20 - fitted with forearm based CAM (controlled active movement) splint
- Exercise program: passive flexion, blocked active extension (PIP/DIP)
- Gentle active flexion
- ROM – PIP 14/36 (/62), DIP –34/40 (/44)
- Treated in the splint for 5/52
Due to the patient living 2.5 hours away and COVID-19 restrictions in place. He was reviewed face to face alternate weeks with a telephone review in between.
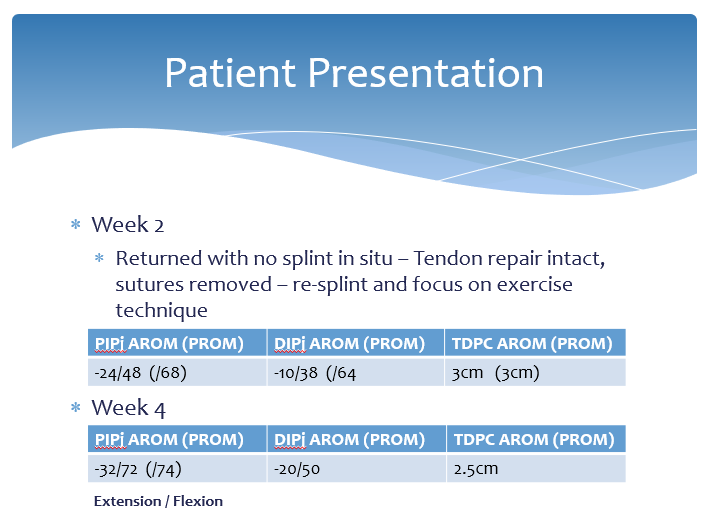
At week 2 the patient returned with no splint in place but luckily the tenson repair was still intact.
At week 4 flexion was starting to improve, however, he was starting to develop a fixed flexion deformity at his PIP joint. This is not uncommon with flexor tendon repairs. The scar was thick and tethered so treatment was focused on scar management. A dorsal extension splint was provided to address the flexion contracture. Home exercises were given for the patient to perform out of his splint from week 5.
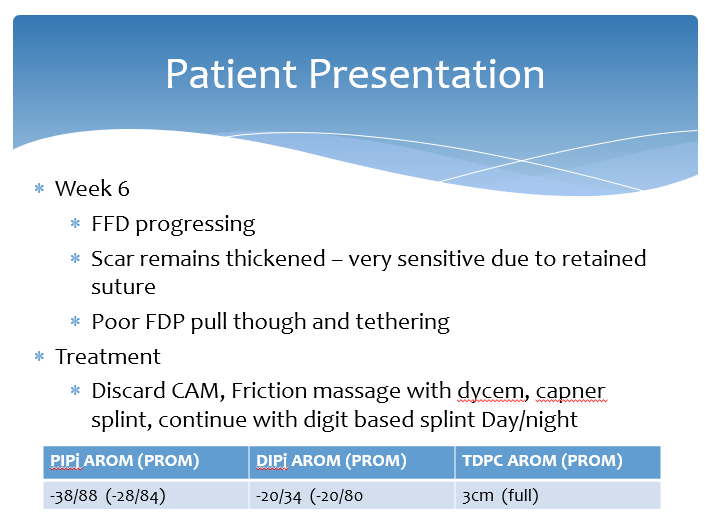
At week 6, despite continuing treatment the fixed flexion deformity was progressing. The scar remained tethered and the pull through of the tendon was limited. Treatment involved self-scar massage, a dyson sheet was provided for friction massage, advice on desensitisation and a specific splint was provided for intermittent use during the day with clear instructions not to flex against it.
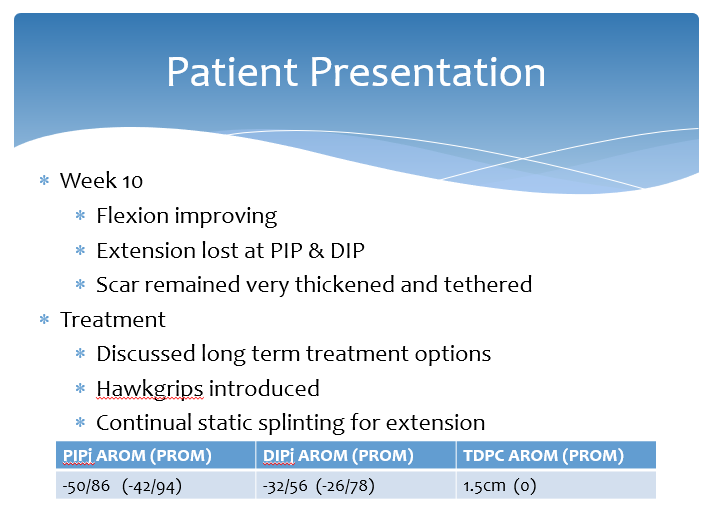
The patient was reviewed at week 10 and long-term treatment options were discussed. Surgical intervention was an option to remove scar tissue and release the joint, however, a decision was made to review the further conversative options including the use of HawkGrips for instrument assisted soft tissue mobilisation.
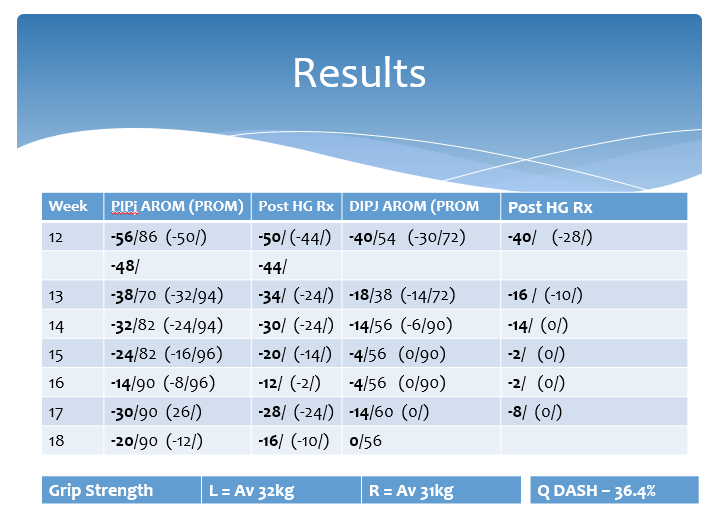
At week 12 post op, the patient had attended weekly appointments for HawkGrips applications, scar management, passive stretching and splint progression.
Progression was made over the weeks of treatment. Both active and passive range of movement improved and the patient maintained the results over a period of time.
Outcome and long term:
- Currently does not require surgery
- Full return to most functional tasks
- Will likely require long term splinting to prevent flexion deformity recurring
- Intermittent monitoring
In conclusion IASTM is a useful tool for the treatment of some flexion deformities in the small joints of the hand. It works well in combination with other therapy treatments such as splinting and home exercise programmes.
Watch the full webinar below:
Patient Background 02:19
Therapy Intervention 03:53
Anatomy of the Flexor Tendons 04:33
Patient Presentation 07:47
Treatment Technique 11:39
Treatment Video using HawkGrips 12:57
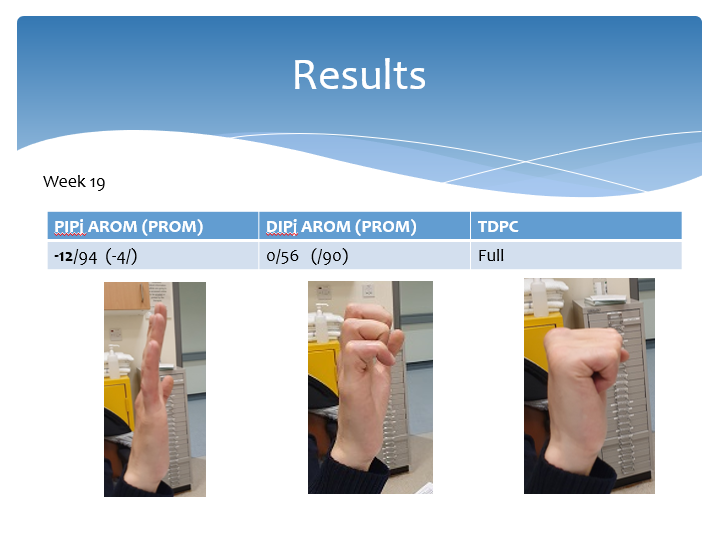
Results 15:42
Week 19 Results 17:07
Outcome & Long Term 17:28
Conclusion 18:09
Q&A Session 19:17
To find out more about the HawkGrips or LymphaTouch, contact Physiquipe on 0161 713 0409 or info@physiquipe.com.